Posted: October 31, 2019
Injury and/or Death to an Unborn Child in a Car Accident
Sadly, in many car accidents involving pregnant women, the unborn fetus can be seriously injured or killed. There can be nothing sadder than for a mother to lose her baby in a car accident caused by the fault of another.
he question as to whether the death of a fetus in utero as a result of a car accident, is a wrongful death claim or an injury claim to the mother is determined by fetal viability.
This means that at the time of the injury, if the unborn child could have lived outside of the mother’s womb then a wrongful death claim can be asserted for the unborn child.
In the case of Werling, ADMX v. Sandy et al. Supreme Court of Ohio 17 Ohio St. 3d 45 (1985), the court was confronted with the issue as to whether an action for wrongful death exists under Revised Code 2125.01 where the decedent was a stillborn fetus. More specifically, the court was asked to determine whether the statutory beneficiaries of an unborn fetus are entitled to damages for the wrongful death of the fetus where both the alleged negligently inflicted injury and the death of the child occurred before birth.
The Court stated that in order to resolve this issue necessarily requires an answer to the question of whether an unborn fetus which dies in a mother’s womb may be considered a “person” for the purpose of the statute under consideration the reasons which follow:
“We answer each of the above queries affirmatively, as long as it is established the fetus was viable at the time of the injury.”
Thus, the Ohio Supreme Court drew a line in the sand, as to whether or not, a wrongful death action could be brought for the death of an unborn fetus. This depends on viability of the fetus..
How Did The Court Determine Viability?
The Court actually recognized that the term “viability” is an elusive one, since not all fetuses arrive at this stage of their development at an identical chronological point in their gestation. The concept may also become increasingly difficult to apply with further developments surrounding the sophisticated medical techniques which allow a child to be conceived outside the mother’s womb.
In the article “Periviable birth (Limit of Viability),” the author Richard A. Ehrenkranz, MD, FFAP and Mark R. Mercurio, MD, MA discussed in detail the subject of periviability, stating:
“Perviability also referred to as the ‘limit of viabilityis defined as a stage of fetal maturity that ensure a reasonable chance of extra uterine survival. With active intervention, most infants born at 26 weeks and above have a high likelihood of survival, and virtually none below 22 weeks will survive. The chance of survival thus increases dramatically over these few weeks, and this crucial time window may be considered the period of periviablity. In addition to the high risk of death in the immediate newbornperiod, children born at the limit of viability have a high risk of permanent disability.
An understanding of both of these risks is essential toparental counseling and decision-making, with regards to attempted resuscitation and provision of life-sustaining measuresin the newborn intensive care unit (NICU).”
Morbidity In Infants At 22 – 25 Weeks Gestation
Significant morbidities that occur in infants between 22 – 25 week gestation that survived the initial neonatal intensive care unit admission include:
Severe intraventricular hemorrhage (IVH);
Periventricular leukomalacia (PVL);
Necrotizing enterocolitis (NEC);
Bronchopulmonary dysplasia (BPD);
Severe retinopathy of prematurity (ROP);
Late onset infection; and
Neurodevelopmental impairment (NDI).
Neurodevelopmental Outcomes
Poor developmental outcome is a major long-term complication of periviable survivors and includes impaired cognition in motor neurosensory deficits. The prevalence of these impairments from cohorts of survivors following birth at 22 to 25 weeks gestation is considerable.
Thus, even a child survives and is born alive, if they sustained a significant injury that impacted them during the 22nd to the 25th week of gestation, there can be severe disability and lifelong physical and mental issues for the child. The child born alive, would have its own cause of action, through its parents for the negligently inflicted injury, as well as the parents for loss of consortiu
This article concluded with the following guidelines for the care of the extremely pre-term infant:
- Below 22 weeks Gestation – Resuscitation is not offered or provided due to the zero or near-zero chance of survival;
- 22.0 – 22.8 Gestation– Resuscitation is offered to parents if there is at least a small chance of survival based on the available information at that time and then it is provided only if requested by the informed parents;
- 23.0 – 23.8 Gestation – Resuscitation is offered to parents, but can be provided or withheld based on the preference of the informed parents;
- 24.0 – 24.8 Gestation – Resuscitation is offered to parents and may be provided or withheld based on the preference of the informed parents. However, if the newborn is predicted to have a greater than 50% chance of survival without NDI, resuscitation is then provided. The likelihood is determined using the NICHD database outcome predictor for patients given mechanical ventilation and using the best obstetrical estimate of GA and estimated fetal weight;
- 25 weeks Gestation & Higher – Resuscitation is provided.
Thus, when a pregnant woman’s unborn child is at least 24 weeks, there is a greater than 50% chance that the child will be able to survive outside the mother’s womb. If the child died in utero or during delivery, the parents as beneficiaries would have a wrongful death claim.
If the child is less than the weeks necessary to conclude a 51% chance of survival for viability, then it would be the mother’s claim for her bodily injury(ies) and the loss of her child would be included in her claim for her injuries.
What Types of Trauma And Physiological Diagnoses are Associated with Traumatic Fetal Deaths?
The article “Fetal Deaths Related to Maternal Injury” authored by Herold B. Weiss, Ph.D, Thomas J. Songer, Ph.D. and Anthony Fabio, Ph.D published in the JAMA Journal, Volume 286, No. 15 studied 240 traumatic fetal deaths during a 3 year study.
It was determined that motor-vehicle crashes were the leading trauma and mechanism (82% of cases; 2.3 fetal deaths per 100,000 live births) followed by firearm injuries (6% of cases) and falls (3% of cases).
The article concluded that motor-vehicle crashes are in fact the leading cause of fetal death related to maternal trauma. It further traced some of the history of fetal deaths.
Trauma during pregnancy has been recognized as an important cause of adverse fetal and maternal outcomes. While early reports described incidents resulting from falls, blows and assaults, later reports increasingly included motor-vehicle crashes.
In this study, the case definition is stated as the following:
“Any fetal death at 20 weeks’ gestation or later affected by an in utero traumatic externally caused injury to the fetus or the mother, excluding birth-related trauma and therapeutic abortion, in which the fetus died before birth, was considered a case of traumatic fetal death.”
Therefore, you can see these authors used a 20-week gestation period as their cut off for the study date. Although, as we have previously seen, this (20 week gestation) would not be enough to cause a wrongful death action in the State of Ohio, it certainly is as a severe and heart wrenching loss to the parents of the unborn child.
This study among traumatic fetal injury death cases with known mechanisms 150 (82%) involved motor-vehicle related crashes, 11 (6%) involved firearms injuries and 6 (3%) were fall related. The age group of the mothers from 15 to 19 had the highest fetus mortality rate.
Placental injury was reported in 100 cases (42%).
How to Safeguard the Fetus in a Car Accident – The Take Away from the Study
The study included that to safeguard fetuses, research and information are needed to gain a better understanding of how to transport pregnant women safely, reduce the crash forces on pregnant women and to reduce other forms of maternal trauma. These measures should consist of the following:
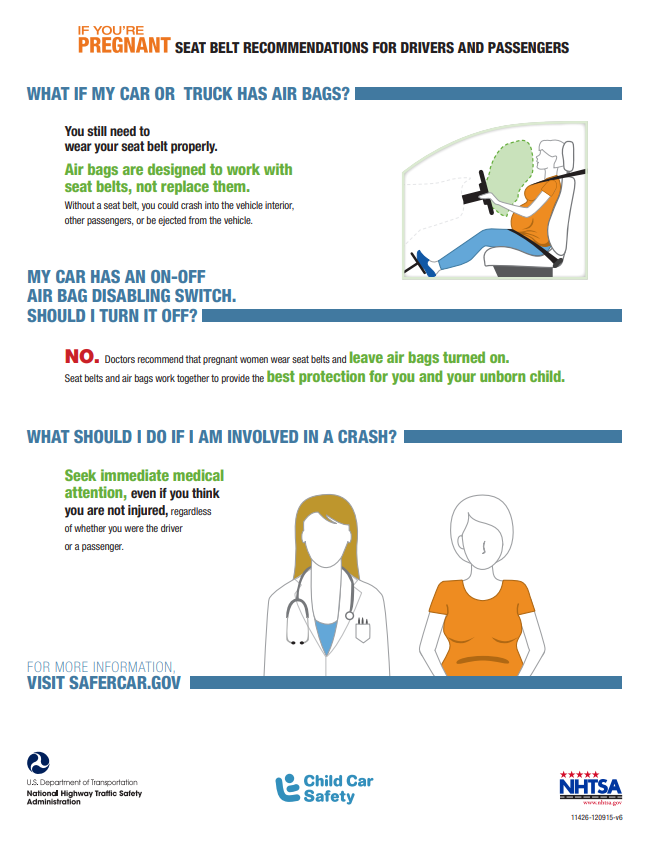
- Incorporating fetal deaths in crash and injury mortality data systems in order to more easily track the problem. There have been many studies now regarding how a pregnant woman should wear her seatbelt. Simply stated, the belt that comes down should be placed over the shoulder and run between the breasts down to the opposite side of the body. The lap belt should be secured below the belly in a way that it fits snuggly across the hip and pelvic bone areas. A lap belt should never be placed over or on the top of the belly.
The below infographic from the National Highway Traffic Safety Administration is instructive about how pregnant women should wear their seatbelt to protect the unborn child.
Effects of Crash Characteristics & Maternal Restraint on Fetal Outcomes in Motor-Vehicle Crashes
In the April 2008 edition, the American Journal of Obstetrics Gynecology published an article titled “Fetal Outcome in Motor-Vehicle Crashes: Effects of Crash Characteristics and Maternal Restraint.” The project was undertaken in order to improve the understanding of factors associated with adverse fetal outcomes of pregnant occupants involved in motor-vehicle crashes. The results of this study were stated as follows:
“Fetal outcome is most strongly associated with crash severity (P<.001) and maternal injury (P=.002).Proper maternal belt-restraint use (with or without airbag deployment) is associated with acceptable fetal outcome (odds ration = 4.5, P = .003). Approximatelyhalf of the fetal losses in motor-vehicle crashes could be prevented if all pregnant women properly wore seatbelts.”
The study concluded that higher crash severity, more severe maternal injury, and lack of the proper use of seatbelts are associated with a high risk of adverse fetal outcome. These results strongly support recommendations that women use properly positioned seatbelts.
This study included subjects starting at 20 weeks gestation and the total crashes investigated ended up being 42 involving 43 pregnant occupants. They also studied 14 other crashes involving pregnant occupants.
Also included in the study were minor complications, such as early contractions, or delivery within 48 hours of the crash at a gestational age of at least 32 weeks. Major complications included placental abruption, uterine rupture or laceration, any direct fetal injury or premature delivery within 48 hours of the crash before 32 weeks gestational age.
In the studied cases, 12 resulted in fetal loss; 11 fetuses survived, but experienced major complications; and the remaining 34 cases had acceptable fetal outcomes. Of the 41 properly restrained pregnant occupants, 12 (29%) experienced adverse fetal outcomes. In addition, of 6 improperly restrained pregnant women, 3 (50%) had adverse fetal outcomes. In terms of unrestrained pregnant women, 8 of 10 (80%) had adverse fetal outcomes. The only 2 acceptable fetal outcomes to unrestrained pregnant women were in crashes with minor severity.
Analysis of Motor-Vehicle Crashes
Fetal outcome is significantly associated with the severity of a crash. Fetal outcome is also strongly associated with the severity of the maternal injury.
The most significant findings revealed that fetal outcomes are related to crash severity, maternal injury and maternal restraint. The study also concluded that airbags did not appear to worsen fetal outcomes.
Currently, the main reason for recommending pregnant occupants use 3-point belts is that protecting the mother is the first step in protecting the fetus, and that using seatbelts significantly reduces risk of injury for the general vehicle-occupant population.
However, the practice of recommending that pregnant patients be instructed to properly use 3-point belts has been questioned by some practitioners because the medical literature contains isolated cases of fetal injuries allegedly caused by seatbelt loading in crashes.
In many of the cases reviewed showed the mechanism of injury and death is placental abruption.
In another significant study published in the Association for the Advancement of Automotive Medicine titled “Injuries to Pregnant Occupants in Automotive Crashes” (Annu Proc Assoc Adv Automot Med. 1998; 42: 57-91.) authored by Klinich Schneider, Moore & Pearlman, the abstract from the study stated:
“Injuries unique to pregnant occupants involved in motor-vehicle crashes include placental abruption, uterine rupture or laceration,and direct fetal injury. The mechanisms and characteristics of these injuries are discussed using examples from a literature review and from recent investigations of crashes involving pregnant occupants. In addition, a review of the relationship between the pregnant driver and automotive restraints and the steering wheel illustrates how injury potential may differ from the non-pregnant occupant.”
Pregnant anatomy is such that as the uterus grows, it pushes the other abdominal organs rearward and upward. The base of the uterus is in close proximity to the lumbar spine.
The placenta is a vascular organ within the uterus that exchanges oxygen, nutrients and waste between the mother and the fetus. This can all be impacted by injury to the fetus.
Placental Abruption
Placental abruption is the most common cause of fetal loss in automotive crashes and occurs in 1 to 5% of minor severity crashes during pregnancy and from 20-50% of severe crashes during pregnancy.
The placental abruption occurs when the placenta detaches from the uterine wall which disrupts the supply of oxygen and nutrients to the fetus.
A partial abruptions can also occur with the possibility of the pregnancy continuing successfully depending upon the degree of placental separation from the uterus.
The inner face between the placenta and the uterus is considered to be weaker than either the uterus or the placenta, and therefore, usually falls before either the uterus or the placenta fails.
In regards to motor-vehicle accidents, the study suggested that placental abruptions may result from high-velocity, low-mass airbag loading or from the compression between the mother’s body and the steering wheel, belt or instrument panel.
A placental abruption may also result from acceleration differentials between the placenta and uterus. Thus, mechanisms of placental abruption may include inertial loading, direct loading by the fetus an excessive shear or tinsel strain.
In the majority of the cases studied regarding placental abruptions, the pregnant occupant was unrestrained (48 out of 69).
The results show that placental injuries can occur to properly belted pregnant occupants and also show that avoiding the belt use during pregnancy may significantly increase the risk of placental abruption and subsequent fetal loss in a crash.
Uterine Injury
Uterine rupture and lacerations are rare during pregnancy, occurring in less than 1% of pregnant trauma cases (Pearlman 1990). Injury to the uterus in automotive accidents occur almost exclusively during pregnancy because it is much larger, extends outside the pelvic cavity and is filled with fluid.
With uterine rupture is very rare, the likelihood of fetal death with such an injury is near 100%.
Direct Fetal Injury
Direct fetal injury is also quite uncommon, occurring in less than 10% of automotive crashes involving pregnant occupants.
During the first 3 months of pregnancy, the uterus is still completely surrounded by the pelvis and is considered an abdominal organ. After the first 3 months, the uterus protrudes out from the abdomen, with the structure of the pregnant abdomen protecting the fetus by encasing it and amniotic fluid, which acts as a shock absorber, to isolate the fetus.
It was determined that direct fetal injury cases normally involve a head injury since the head is the largest organ on the unborn child.
Other negative outcomes and other common occurrences in premature delivery in which the infant often has a low birth weight and can suffer from neonatal respiratory distress syndrome due to the fact that its lungs are not fully developed. Both of these factors can lead to health problems and disabilities throughout the child’s life.
Even if the fetus is close to full term, maternal involvement in a crash can lead to an emergency caesarean delivery which poses a higher risk to the mother and neonate.
Contractions often begin after an accident, sometimes requiring drug intervention to prevent early delivery.
Crashes involving pregnant occupants occasionally result in stillborn births without any visible injury responsible for the loss.
The significant conclusions in the article are as follows:
“While placental, uterine and fetal injuries may
occur with properly belted occupants, the
majority of the cases involving these injuries
are to unrestrained occupants.”
Distinguishing Characteristics
These cases with completely positive fetal outcomes was when proper restraint was used by the mother. All pregnant women involved in crashes, even minor crashes, should immediately seek medical attention. In most cases with fetal loss, the mother sustained only minor or no other injuries other than placental, uterine or fetal damage.
Although this article seems to suggest that proper seatbelt use is effective in preventing pre-natal injuries, I have represented multiple properly restrained women who have either sustained significant injury to the fetus requiring emergency cesarean section and/or death of the fetus.
A Mechanism of Placental Abruption
An article in the Obstetrical and Gynecological Survey entitled “Trauma During Pregnancy: Maternal and Fetal Injury” authored by Warren M. Crosby discusses the causal relationship between the traumatic event and the subsequent pregnant injury.
In terms of premature separation of the placenta, the mechanism is not entirely clear. The placenta does not contain elastic tissue and possesses very little capability to expand or contract. Conversely, the uterine wall is elastic. During the impact sequence, the unrestrained body decelerates against some part of the vehicle or if ejected, against the earth, outside of the vehicle or into other objects.
The uterus flattens against that part of the abdomen that decelerates first, then vertical waves cause rapid elongation and shortening of the long axis of the uterus, shearing placental attachments.
Thus, premature separation of the placenta might be an expectant concomitant of sudden deceleration in late pregnancy, yet it occurred to a clinically recognizable degree in less than 6% of the victims with severe collision.
Trauma is universally considered among the possible causes for premature separation of the placenta. With the uterus, fetus and placenta, the belted mother is subjected to part of the force of deceleration in every severe collision. It was felt that possibly the overall benefit of a lap belt may be offset by the increasing injury brought about by the jack-knifing and the mother’s body over the lap belt.
This is apparently the reason the 3-point restraint system is suggested to reduce the frequency of maternal and fetal injury by distributing the decelerating force more evenly and by preventing forward flexion.
The study’s suggested criteria about a probable relationship between a traumatic event and subsequent onset of premature labor as follows:
The study also states these factor suggest a causal relationship between a traumatic event and subsequent premature separation of the placenta:
- The pregnancy should have been progressing normally prior to the traumatic event;
- There should be no evidence of factors known to predispose to placental separation, including previous vaginal bleeding, hypertension or toxemia of pregnancy, or acquired or congenital uterine deformities;
- The signs and symptoms of placental separation, including vaginal bleeding, uterine tetany, fetal death, and uterine tenderness, should have begun within 48 hours of the traumatic event and have terminated the pregnancy shortly thereafter; an
- The diagnosis of placental separation should be confirmed by the present of an adherent clot or a depression on the maternal surface of the placenta.
Conclusion For Pregnant Women and Car Accidents - How To Protect Yourself and Your Unborn Child
There is no doubt that fetal injury that can occur as a result of a car accident. The risk of fetal injury appears to be lessened by the proper use of a 3-point restraint, including a lap belt and a shoulder belt with the lap belt being worn around the bottom of the abdomen near the hips and not over the abdomen.
Whether a fetal death is a wrongful death in the State of Ohio or an injury to the mother is determined by whether or not the fetus is viable. This is a factual matter that deals primarily with the weeks of gestation, as well as other factors.
The bottom line is that when any pregnant woman is any type of car accident, she should immediately go to the emergency room to be checked out and evaluated in order for a medical determination of the unborn child’s welfare. This is especially important since there can be significant trauma to the fetus without the mother noticing or incurring severe injury.
If you are pregnant and injured in a car accident and would like to know your rights in the State of Ohio, please call Anthony D. Castelli, greater Cincinnati personal injury attorney near me at 513-621-2345 for a free consultation.
Use this tool to determine outcomes for survival, survival without profound neurodevelopment impairment, survival without moderate to severe neurodevelopment impairment, death, death or profound neurodevelopmental impairment, death or moderate to severe neurodevelopmental impairment based upon gestational age, birth weight, sex, singleton birth and use of corticosteroids.
Author: Anthony Castelli personal injury trial lawyer
513-621-2345